PPH-POSTPARTUM HEMORRHAGE
➡️ PPH
PPH is excessive bleeding of > 500 ml from the genital tract
Any time following the baby’s birth up to 6 weeks after delivery
98% of PPH occurs within 24 hours of delivery
TYPES OF PPH
? This is the leading cause of maternal mortality. It is obstetric hemorrhage
A woman bleeds heavily, most often immediately after giving birth.
A woman somewhere in the world dies every 4 minutes from this kind of complication.
A crucial role for nurses and midwives is to prevent, detect and manage postpartum hemorrhage
We save lives by being knowledgeable and taking quick action when mothers are bleeding too much
Who is at risk for PPH?
All women are at risk
If sick, anemic, malnourished—she has increased risk of being affected with a small amount of blood loss
Blood can be liquid or in clots
The bleeding can be slow and constant or a large amount at once.
The loss of 500 ml or less can be life threatening
To Prevent PPH:
Active Management of third Stage of Labor (AMSTL)
World Health Organization endorsed intervention
Helps the uterus to contract and prevents PPH
It is advised for all women at delivery
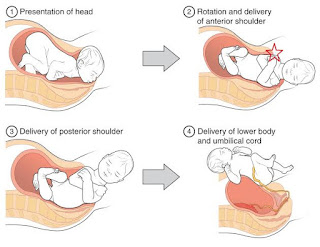
➡️ AMSTL Steps:
-Rule out the presence of another baby
– With 1 minute after the baby’s birth– administer 10 IUs of oxytocin IM to anterior thigh muscle
– Wait for the to uterus separate.
– Then perform controlled cord traction with counter-traction to support the uterus
– Deliver the placenta
– Massage the uterus
?WHY AMTSL?
Speeds the delivery of the placenta
Increases uterine contractions
Prevents uterine atony (and therefore PPH!)
Within one minute!
Administer a uterotonic medicine within one minute after the baby is born
In Tanzania: 10 IUs of OXYTOCIN IM
Another option is Misoprostol 600 mcg orally
☑️ What are the three signs of placental separation?
The Three Signs of Placental Separation:
(1) Lengthening of the cord
(2) Gush of blood
(3) Fundus rises to globular
How Can I Check for Placental Separation?
Placenta
Separation
Steps
✓ Controlled Cord Traction
✓ During a contraction, perform CCT
✓ Support and stabilize the uterus by applying counter traction
✓ Once the placenta is out—the uterus can contract!
✓ CCT involves pulling with a firm, steady tension on the cord in a downward direction during contractions.
✓ CCT helps the placenta descend into the vagina. This facilitates its delivery. The uterus cannot contract efficiently if the placenta is still inside.
✓ When performing CCT, the uterus needs to be supported or guarded to prevent uterine inversion.
✓ Applying counter pressure on the lower segment of the uterus in an upward direction towards the woman’s head.
✓ Perform CCT ONLY during a contraction.
How to Deliver the Placenta
In removing the placenta, take steps to reduce the risk of tearing the placenta or membranes
Use both hands to hold the placenta and turn it gently
The membranes will twist like a rope
Put the placenta into a basin
Examine it to make sure that it is complete
Massage the uterus immediately after delivery of the placenta and membranes until it is firm.
If there is excessive bleeding, massage the uterus.
Massaging the uterus stimulates uterine contractions and helps to prevent PPH.
After you stop massage, it is important to make sure that the uterus does not relax again.
Teach the woman how to massage her own uterus and ask her to call if her uterus is soft.
Delayed Cord Clamping
After the baby’s birth, wait to 2 to 3 minutes to clamp and cut the cord.
Wait 2-3 minutes or until the cord stops pulsating.
Studies show this is helpful to all babies.
In low birth weight or premature infants, delayed cord clamping is important.
Skin to Skin
Natural Oxytocin, Natural Warmer!
Managing the Third Stage of Labor
What if there is excessive bleeding?
How will we know it is excessive?
How much is 500 ml?
500 ml = approximately
soaked khangas
PPH is excessive bleeding
The patient will have symptoms!!
-She will show signs of shock or low blood volume
-Lightheaded, palpitations, diaphoresis, confusion
-Low BP and increased pulse
-Low urine output
-Decreased O2 saturation
Effect of blood loss depends on mother’s general wellbeing and pre-delivery hemoglobin
Signs of PPH?
Signs of shock or low blood volume
– Pallor
– Rising pulse rate
–Falling blood pressure
– Rise in respiratory rate
– Change in level of consciousness – the mother may become restless or drowsy
– An enlarged uterus filled with blood
– The uterus feels soft and spongy on palpation
* There may be little or no visible loss of blood
What if there is excessive bleeding?
?THE CAUSES OF PPH
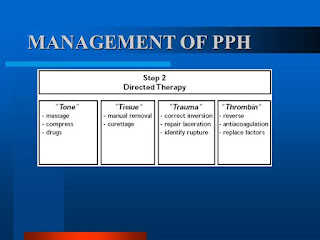
What are the possible causes? (4-T’s)
1)T–
2)T–
3)T–
4)T–
1.Tone (uterine atony) – MOST COMMON 70%
2.Tissue (retained tissue) – 10%
3.Trauma from tears – 20%
4.Thrombin (clotting problem) – less than 1%
TONE – UTERINE ATONY
Atony is the most common cause of PPH
The uterus does not contract after delivery
To stop the bleeding of the uterine blood vessels, the uterus must contract
Otherwise, the vessels will continue to pump blood into the empty uterus
Prevention: AMSTL
Risk Factors for Uterine Atony
-Prolonged or obstructed labour
-Mismanagement of third stage of labour
-Full bladder (uterus deviates to the right & can’t contract!)
-Antepartum haemorrhage – abruption, placenta previa
-Stretched uterus – twins, polyhydramnios, macrosomia
-General and epidural anaesthesia
-Chorioamnionitis
-Severe pre-eclampsia/eclampsia with coagulation defects
-Prior hx of PPH due to atony – 10% risk of recurrence
-Use of oxytocin for labour induction or augmentation
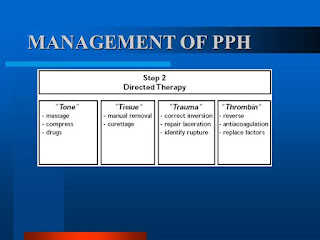
?THE MANAGEMENT OF PPH
What is the management for PPH after placenta has been delivered?
Remember the four Ts:
Tone
Tissue
Trauma
Thrombin
PPH Management after Delivery of Placenta:
- Shout for help
- Massage uterus and expel clots. Maintain massage.
- Give another dose of oxytocin 10 units IM or Misoprostol 1000mcg rectally or 800 mcg under tongue.
- Start 2 IV infusions with 14 or 16 gauge. Run NORMAL SALINE or Ringers Lactate.
- In one IV, run 20 units/liter of oxytocin at 60 drops per minute. Once bleeding slows decrease to 30 drops/min.
- If bleeding continues, add another 20 units of oxytocin to the bag
- Run the other IV wide open!
- Empty the bladder!
- If heavy bleeding continues–apply bimanual compression
- Get haemoglobin and cross match blood
MIDWIFERY COURSE PDF NOTES
11. Cord Prolapse and Presentation
13. Pre-eclampsia and Eclampsia
15. Risk factors occuring During Pregnancy